
Tandem (double autologous) transplantsĭoing 2 autologous transplants in a row is known as a tandem transplant or a double autologous transplant. The need to remove cancer cells from transplanted stem cells or transplant patients and the best way to do it continues to be researched. For instance, lenalidomide (Revlimid ®) may be used in this way for multiple myeloma. After transplant, the patient gets anti-cancer drugs to get rid of any cancer cells that may be in the body.

This could increase the risk of infections or bleeding problems.Īnother treatment to help kill cancer cells that might be in the returned stem cells involves giving anti-cancer drugs after the transplant. This may cause your body to take longer to start making normal blood cells, and you might have very low and unsafe levels of white blood cells or platelets for a longer time. A possible downside of purging is that some normal stem cells can be lost during this process. While this might work for some patients, there haven't been enough studies yet to know if this is really a benefit. To help prevent any remaining cancer cells from being transplanted along with stem cells, some centers treat the stem cells before they’re given back to the patient.
Getting rid of cancer cells in stem cells saved for autologous transplants Doctors can use autologous transplants for other diseases, too, like systemic sclerosis, multiple sclerosis (MS), and systemic lupus erythematosis (lupus).

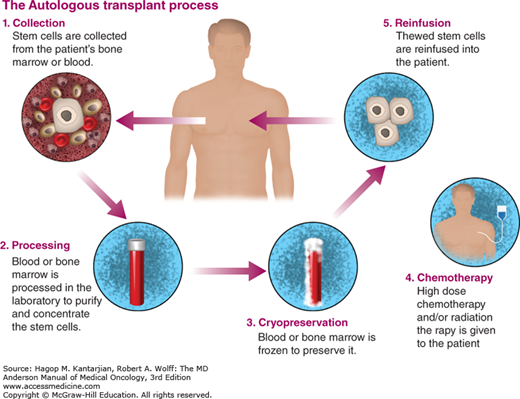
It’s sometimes used for other cancers, like testicular cancer and neuroblastoma, and certain cancers in children. This kind of transplant is mainly used to treat certain leukemias, lymphomas, and multiple myeloma. This means the cancer cells were able to escape attack from your immune system before, and may be able to do so again. Another disadvantage is that your immune system is the same as it was before your transplant. A possible disadvantage of an autologous transplant is that cancer cells might be collected along with the stem cells and then later put back into your body. Also, autologous transplants can’t produce the “graft-versus-cancer” effect. The grafts can still fail, which means the transplanted stem cells don’t go into the bone marrow and make blood cells like they should. Risks of autologous stem cell transplant: When you get your own stem cells back, you don’t have to worry about them (called the engrafted cells or the “graft”) being rejected by your body. (You can learn more about this process at What’s It Like to Donate Stem Cells?) After you get high doses of chemo and/or radiation as your myeloablative therapy, the stem cells are thawed and given back to you.īenefits of autologous stem cell transplant: One advantage of autologous stem cell transplant is that you’re getting your own cells back. Your stem cells are removed from either your bone marrow or your blood, and then frozen. In this type of transplant, the first step is to remove or harvest your own stem cells. The stem cells in allogeneic transplants are from a person other than the patient, either a matched related or unrelated donor. The stem cells in autologous transplants come from the same person who will get the transplant, so the patient is their own donor. They are named based on who donates the stem cells. The goal is that over time, the transplanted cells settle in the bone marrow, begin to grow and make healthy blood cells. Stem cells are given into a vein, much like a blood transfusion. Soon after treatment, stem cells are given (transplanted) to replace those that were destroyed.

This is called myeloablation or myeloablative therapy. This treatment also kills the stem cells in the bone marrow. In a typical stem cell transplant for cancer, very high doses of chemo are used, sometimes along with radiation therapy, to try to kill all the cancer cells. They can all be called hematopoietic stem cell transplants. Depending on where the stem cells come from, the transplant procedure may be called: Stem cell transplants are used to give back stem cells when the bone marrow has been destroyed by disease, chemotherapy (chemo), or radiation.


 0 kommentar(er)
0 kommentar(er)
